MALAWI PROFILE:- SUMMARY ON OPEN BUDGET SURVEY AND HEALTH PROFILE
OPEN BUDGET SURVEY (OBS)
i.Transparency
Malawi’s transparency score is the second lowest in the Southern Africa Region only scoring higher thatn Zambia. The transparency score has declined from a high of 65 percent in 2015 to a low of 20 percent in 2021 rolling back the gains made over the years. The government has not only reduced the number of publicly published budget documents but also their comprehensiveness. Crucial budget documents including the Enacted Budget, Year End Reports and Audit Reports have only been developed for internal use. The government needs to timely publish and publicly avail comprehensive budget documents.
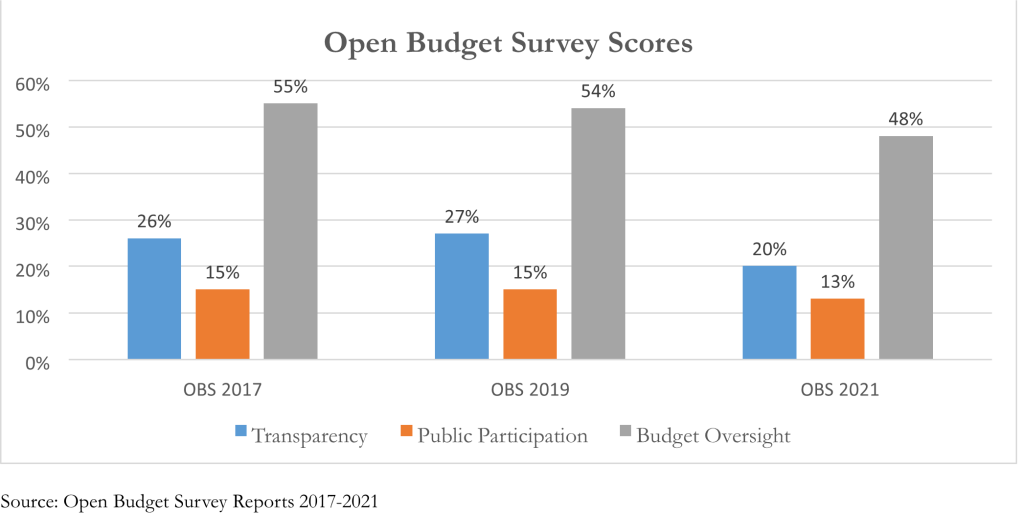
ii. Public Participation
Malawi provides insufficient opportunities for citizens to engage in the budget process. Its public participation score reduced to 13 percent in 2021 from 15 percent in 2019. Citizens are only provided the opportunity to engage in the budget process during formulation of budgets. They do not engage with Parliament during budget approval, Executive during budget implementation and Supreme Audit Institution (SAI) during audit. There’s need to provide citizens with the opportunity to engage with decision makers across the budget process to ensure that their priorities are captured in the budgets before they are approved; they are effectively implemented within the year and provide their feedback on public expenditure impact during oversight/audit.
iii. Budget Oversight
Both Parliament and SAI in Malawi provide limited budget oversight. The overall budget oversight scores declined from 55 percent in 2017 to 48 percent in 2021. Within this period, the extent of budget oversight provided by the legislature declined from 73 percent to 50 percent. On the other hand, the budget oversight provided by SAI remained constant at 44 percent. There is need to enhance budget oversight to ensure public expenditure responds to citizen needs in a cost-effective manner. Additionally, there’s need to ensure independence of the SAI by requiring legislative/judicial approval before removal of the Head of SAI.
HEALTH PROFILE
Health Expenditure
The per capita health spending in Malawi in US$ million constant (2020) has increased from US$ 17 in 2007 to a high of US$ 40 in 2013 before declining to US$ 33 in 2020. The bulk of this spending has been funded through government transfers and external aid as shown below:
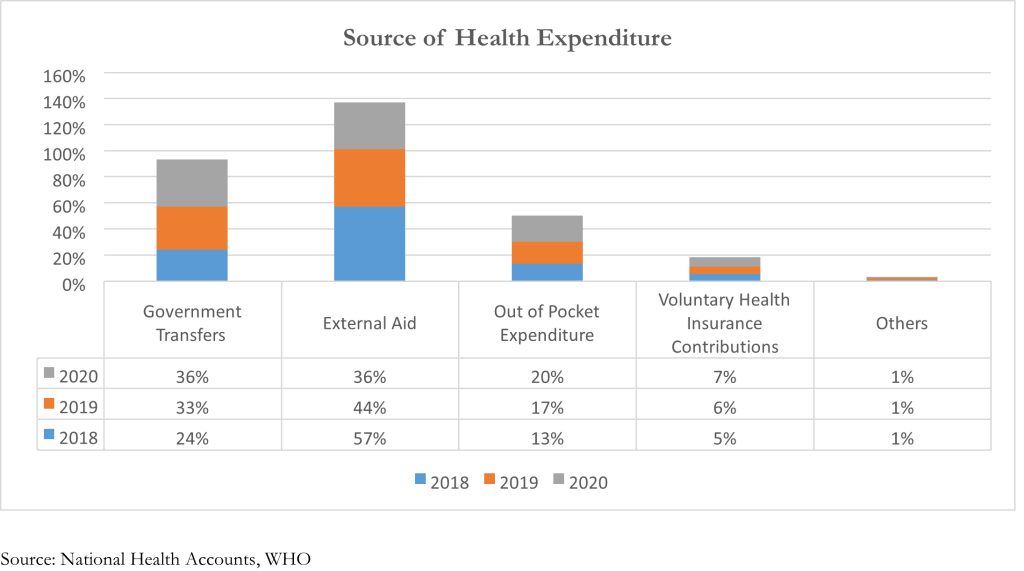
The proportion Health Expenditure funded through external aid has been on a decline from 2018 to 2020, i.e. from 57 percent to 36 percent. In real terms, this has declined from US$ 436 million to US$ 232. To bridge this decline, proportion of health expenditure funded through government transfers have increased from 24 percent to 36 percent within the same period (US$ 186 million to US$.232 million) Additionally, the out of pocket (OOP) expenditure has increased from 13 percent to 20 meaning that Malawians are spending more of their resources to fund healthcare i.e. per capita OOP in US$ has increased from US$ 4.74 in 2018 to US$ 6.44 in 2020. This increases their risk of being pushed into poverty because of unexpected illness that requires them to use up their life savings, sell assets, or borrow.i
Current Health Expenditure as a percentage of GDP has been on a decline from 2016 at 7.73% of GDP to 5.43% of GDP in 2020. This shows that the health sector has not been prioritized relative to other sectors in the economy. In real terms, the current health expenditure in US$ million constant (2020) declined from US$ 760 million to US$ 639 million. This is mainly attributed to the decline in external aid funding as shown above.
Additionally, official health funding (government and external funds) per capita has declined in recent years from US$ 30.24 (US$ 9.04 from government and US$ 21.24 from donors) in 2018 to US$ 23.91 (US$ 11.96 from government and US$ 11.95 from donors) in 2020. This is below the recommended international official health funding benchmark of US$ 86 per capita that is required to achieve UHC, as recommended by McIntyre and Meheus (2014).ii
Primary Healthcare
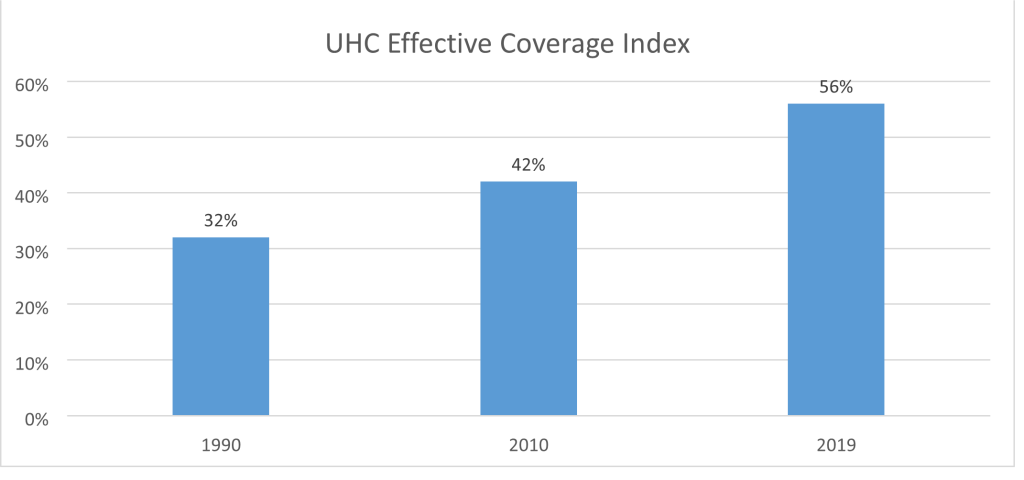
Enhancing access to primary healthcare provides a feasible route to achieving Universal Health Care Coverage. Malawi has made steady strides towards increased UHC coverage i.e. UHC effective coverage index has increased from 32 percent in 1990 to 56 percent in 2019. This indicates increased service coverage across the population health needs that could contribute to improved health outcomes.iii
Source: Global Burden of Disease Study
Between 2009 and 2019, the two leading diseases that caused the most deaths in Malawi were HIV/AIDS and neonatal disorders. On the other hand, malaria moved from being the third highest cause of death to the sixth and its position taken by lower respiratory infections as the third leading cause of death. During this period, malnutrition, unsafe sex and air pollution were identified as the risk factors that drive the most deaths and disability.
Additionally, Malawi has made significant progress in addressing Child (under-5) and infant (under1) mortality. The under-5 mortality (death per 1,000 live births) declined from 200.7 in 1990 to 58.4 in 2019. Similarly, under-1 mortality notably declined 113.7 to 40.8 indicating improved health outcomes for these groups.
i Meheus and Di Mclntyre (2017). ‘Fiscal space for domestic funding of health and other social services’. National Library of Medicine ii Di McIntyre and Filip Meheus (2014). ‘Fiscal Space for Domestic Funding of Health and Other Social Services’. Chatham House
iii Vollset et al (2020). ‘Fertility, mortality, migration and population scenarios for 195 countries and territories from 2017 to 2100: a forecasting analysis for the Global Burden of Disease Study.’ The Lancet, 396(10258), P1285-1306